As part of Aetna’s commitment to enhancing access to evidence-based addiction treatment options for its members, medication-assisted treatment (MAT) is available for those with opioid use disorder. MAT includes medications designed to help suppress cravings and lessen withdrawal symptoms, along with opportunities to seek additional support and help in the community.
According to a study published in the American Journal of Managed Care, people who don’t follow medication-assisted treatment are more likely to relapse. The June 2017 study, which Aetna participated in, was spurred by a separate study Aetna conducted in the 2010 that looked at 2,135 members and found medication-assisted treatment associated with lower utilization of services.
“For those individuals with opioid use disorder, the risk of dying has been shown to drop by more than half when treated with medication-assisted therapy,” said Dan Knecht, M.D., M.B.A, vice president and head of Clinical Strategy and Policy at Aetna. “This is the rationale behind why we are promoting its appropriate use in our opioid strategy.”
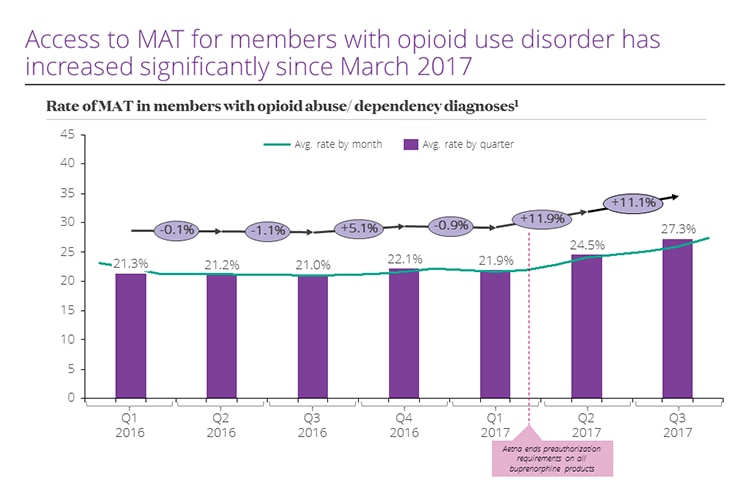
In 2017, Aetna announced its commitment to increase the percentage of Aetna members with opioid use disorder treated with medication-assisted therapy or other evidence-based treatment by 50 percent by 2022. Aetna also was one of the first insurers to end preauthorization requirements on all buprenorphine products, which is used to treat opioid addiction. The move (marked by the purple dotted line below) helped significantly increase access to these important treatments:
“We’re working to prevent misuse and abuse, intervene when we identify at-risk behavior and support those who are addicted through evidence-based treatments,” said Hal L. Paz, M.D., M.S., executive vice president and chief medical officer for Aetna. “Medication-assisted treatment can be extremely beneficial for individuals with opioid use disorder.”
Despite compelling evidence that MAT supports patients’ journeys to recovery, stigma exists. Additionally, the need for prescribers to obtain specific training and licensure before prescribing MAT has resulted in significant access challenges for many patients.
“We are working with various stakeholders in the health care ecosystem, including the National Institutes of Drug Abuse, to educate providers about this program,” said Knecht.
Aetna’s Chief Medical Officer of Behavioral Health, Mark Friedlander, M.D., M.B.A., added that medication-assisted treatment is designed specifically to reduce cravings and the severity of withdrawal symptoms.
“People that use medication-assisted treatment as prescribed are not getting high and they’re not using it recreationally,” he explained.
The medication, Friedlander added, is just one component to medication-assisted treatment. Prescriptions are also paired with counseling and therapies, as well as access to support services personalized to each person.
Paz, Knecht and Friedlander agreed that if everyone works together they’re hopeful stakeholders can collectively help combat the ongoing crisis in the country, with MAT a cornerstone treatment for many with opioid use disorder.